Secondary lung cancer
This information is about secondary cancer in the lung. The term ‘secondary cancer in the lung’ describes the situation where cancer cells have spread to the lungs from a cancer that began elsewhere in the body. The original cancer is described as a primary cancer, and when it spreads this is referred to as secondaries or metastases.
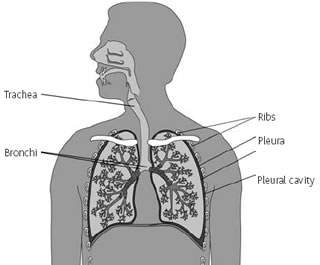
The lungs
The lungs are a pair of organs in the chest that are responsible for breathing. When you breathe in, air passes from your nose or mouth through the windpipe (trachea) into one of the two airways (bronchi) which enter the lungs. These airways divide to form smaller tubes, at the end of which are millions of tiny sacs. It is here that oxygen is absorbed from the air and passes into the bloodstream to be circulated around the body. The lungs are surrounded by a protective lining that consists of two membranes called the pleura.
Cancer in the lung
Cancer can develop in the lungs in two ways. It can start in the lung (primary lung cancer), or it can spread there from a primary cancer elsewhere in the body. If a cancer spreads to the lungs from another part of the body, this is known as secondary or metastatic lung cancer.
Cancerous tumours are made up of millions of cells. Some of these cells may break away from the primary cancer and travel in the bloodstream or the lymphatic system to another part of the body, in this case the lungs. Although any type of cancer can spread to the lung, the most common types are cancer of the large bowel (colon and rectum), breast, ovary, testicle, stomach, gullet (oesophagus), kidney (renal) and a type of skin cancer called malignant melanoma.
Signs and symptoms
The symptoms of a secondary lung cancer may be quite distressing and can include:
- a cough that does not clear up
- breathlessness
- coughing up blood-stained phlegm (sputum)
- pain or discomfort in the chest.
Many of these symptoms are similar to those of a primary lung cancer. They are more commonly caused by conditions other than cancer, such as a chest infection, but you should see your doctor if you have any of these symptoms. A doctor may suspect a secondary lung cancer if there has been a previous diagnosis of cancer and you have some of these symptoms, particularly if they don’t respond to other treatment such as antibiotics.
Sometimes secondaries or metastases are found before a primary cancer has been diagnosed. Occasionally it may not be possible to find the original cancer – this is called an ‘unknown primary’.
Diagnosis
A number of tests may be done to diagnose a secondary lung cancer, including:
Chest x-ray
CT (computerised tomography) scan This is a sophisticated type of x-ray that builds up a three-dimensional picture of the inside of the body. The scan is painless but takes longer than an ordinary x-ray (up to 30 minutes). CT scans use a small amount of radiation, which will be very unlikely to harm you and will not harm anyone you contact.
Special liquids are often used to allow particular areas of the body to be seen more clearly on the scan. They may be given as a drink or an injection, or both. You will probably be able to go home as soon as the scan is over.
MRI (magnetic resonance imaging) scan This is similar to a CT scan, but uses magnetism instead of x-rays to build up cross-sectional pictures of your body. During the test you will be asked to lie very still on a couch inside a long chamber for up to an hour.
Biopsy Sometimes the doctors need to carry out a biopsy. This is usually done in the x-ray department, most commonly during a CT scan. A local anaesthetic is used to numb the area before a needle is inserted to remove a small piece of tissue. The sample can then be examined under a microscope. The biopsy may be slightly uncomfortable but only takes a few minutes.
A secondary lung cancer may also cause fluid to collect in the space between the two membranes (the pleura) that surround the lungs. This is known as a pleural effusion. If this happens it may be possible to remove some of the fluid and examine it for cancer cells.
When the cancer cells are examined, the doctors can tell that it is a secondary lung cancer because the cells look like the cells from the original cancer. For example, if a stomach cancer has spread to the lungs, the cells would look like stomach cells rather than lung cells.
Treatment
The treatment for a secondary lung cancer depends on the primary cancer. Often chemotherapy or hormonal treatment can be given to reduce and control lung secondaries.
Surgery to remove the secondary lung cancer may be possible for a small number of people. This may be an option only if the primary cancer has been controlled and there is no evidence of the cancer having spread anywhere else in the body. It also requires the cancer to be affecting just one small part of the lungs, which is easy to get at and not attached to important blood vessels or nerves.
A short course of radiotherapy may be given to relieve some of the symptoms of the secondary lung cancer, such as pain, breathlessness or coughing up blood (haemoptysis).
If the cancer is causing a blockage in the windpipe or one of the large airways, laser therapy may be used to burn the tumour out of the airway. This may relieve some of the symptoms, though it does not destroy the cancer completely. If the cancer is causing pressure on structures close to the windpipe a small tube called a stent may be inserted to hold the windpipe open. The stent can remain in the lung permanently and does not cause any problems.
A special form of internal radiotherapy called endobronchial radiotherapy or brachytherapy may be given when the tumour is blocking one of the airways. A thin tube (catheter) containing radioactive material is placed close to the tumour using a bronchoscope (a thin, flexible tube used to examine the inside of the airways). Usually only one session of treatment is needed.
Coping with the symptoms
The symptoms of a secondary lung cancer can affect a person’s day-to-day life and can be distressing.
It can help to note down your main symptoms so that when you see the doctor you can discuss each in turn.
Breathlessness This is a common and frightening problem which can affect all aspects of your life. The distress caused by being breathless can be partly relieved by medication and activities such as muscle relaxation.
Fluid on the lung A secondary lung cancer may cause a build-up of fluid between the two membranes (the pleura) that surround the lungs. This is known as a pleural effusion. The fluid puts pressure on the lung and may cause breathlessness, a cough and a dull aching pain. These symptoms can be relieved by carefully draining the fluid using a syringe and needle or a tube. Sometimes it is not possible to drain the fluid as it can collect in a number of small pockets rather than in one place. The fluid tends to build up again, so a chemical may be inserted into the space between the pleura to try to prevent it from recurring. This procedure is called pleuradesis and occasionally it may be done surgically for better effect. However, this is more complicated and will only be suitable for patients who are otherwise very fit.
Cough and chest pain These can usually be relieved using medicines, which your doctor can prescribe.
Fear of choking People who are experiencing problems with breathing may have a fear of choking. However, this is very unlikely to happen.
Coughing up blood (haemoptysis) It is not unusual to notice some streaks of blood in your phlegm if you have secondary lung cancer. If you have larger amounts of blood let your doctor know so he or she can plan specific treatment (such as radiotherapy) to control it.
Research trials
Research into treatments for secondary cancers in the lung is ongoing and advances are being made. Cancer doctors use clinical trials to assess new treatments. Before any trial is allowed to take place, an ethics committee must have approved it, and agreed that the trial is in the interest of patients.
You may be asked to take part in a clinical trial. Your doctor must discuss the treatment with you so that you have a full understanding of the trial and what it means to take part. You may decide not to take part or to withdraw from a trial at any stage. You will then receive the best standard treatment available.
CancerBACUP’s section on cancer research trials, explains how clinical trials are set up and answers common questions that people have about them.
Your feelings
You may have many different emotions, including anger, resentment, guilt, anxiety and fear. These are all normal reactions and are part of the process many people go through in trying to come to terms with their illness.
CancerBACUP has further information on the emotional effects of cancer and how to deal with them. There is also information which discusses how to deal with the practical issues that arise when cancer comes back.
References
This section has been compiled using information from a number of reliable sources including;
- Oxford Textbook of Oncology (2nd edition). Souhami et al. Oxford University Press, 2002.
- Cancer and Its Management (4th edition). Souhami and Tobias. Oxford Blackwell Scientific Publications, 2003.
- Oxford Textbook of Palliative Medicine (3rd edition). Doyle et al. Oxford University Press, 2004.
For further references, please see the general bibliography.
Page last modified: 02 November 2005